
The narrative surrounding HIV has undergone a dramatic transformation. Once synonymous with rapid decline and inevitable mortality, the disease can now be managed as a chronic condition, thanks in no small part to the crucial role of laboratory diagnostics. This blog post delves into the scientific underpinnings of how lab tests have revolutionized the approach to HIV treatment.
Learn More About HIV Diagnosis
Early Detection: The Foundation for Success:
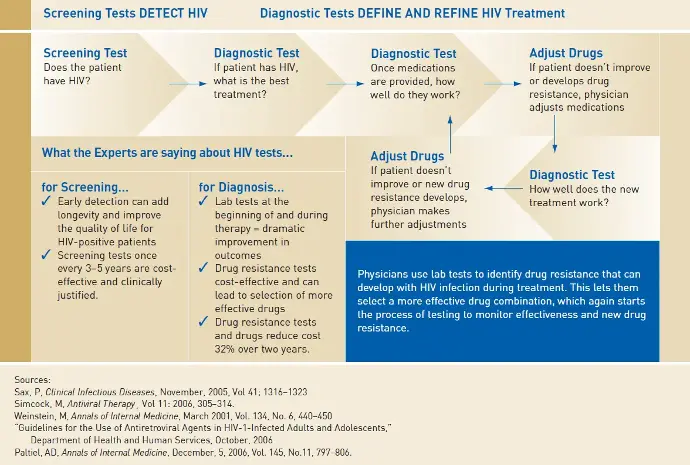
The cornerstone of effective HIV management lies in early identification. Screening tests, routinely recommended every 3-5 years, act as the first line of defense. These tests, employing techniques like enzyme-linked immunosorbent assays (ELISA) or rapid diagnostic tests, detect the presence of HIV antibodies, allowing for prompt intervention. Early detection translates to earlier initiation of antiretroviral therapy (ART), a critical factor in preserving immune function and preventing opportunistic infections.
A Symphony of Diagnostic Tools: Guiding Treatment Decisions:
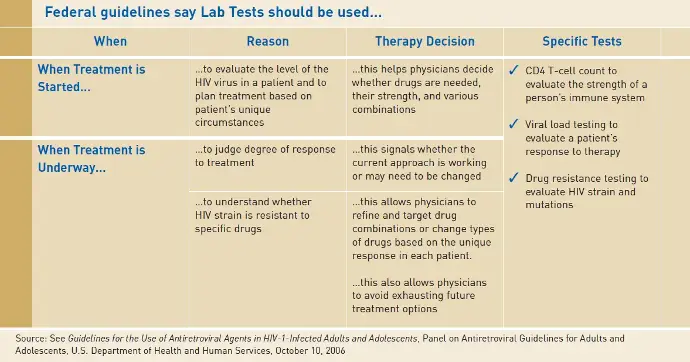
Following a confirmed HIV diagnosis, a comprehensive battery of laboratory tests paints a detailed picture of the viral landscape and immune status. These tests provide invaluable data for crafting a personalized treatment plan:
- CD4+ T-lymphocyte (CD4) Count:
This test quantifies a specific type of white blood cell, a critical component of the immune system. A low CD4 count signifies a weakened immune response, informing treatment decisions regarding the urgency of ART initiation and potential prophylaxis against opportunistic infections.
- Plasma HIV RNA Viral Load:
This test measures the circulating level of HIV viral RNA, a direct indicator of viral activity. A high viral load suggests potential treatment failure, prompting modifications to the ART regimen.
Precision Medicine in Action: Unveiling Drug Resistance:
HIV, a notorious shapeshifter, possesses a remarkable ability to mutate, potentially rendering existing therapies ineffective. Here's where drug resistance testing steps in. Techniques like genotypic resistance assays and phenotypic assays analyze the viral strain for mutations conferring resistance to specific drugs. This information empowers clinicians to:
- Optimize Drug Selection:
By identifying resistant mutations, doctors can tailor the initial ART regimen, minimizing the risk of early treatment failure.
- Dynamic Treatment Adjustments:
As the virus evolves, resistance testing guides adjustments to the ART regimen, ensuring continued viral suppression.
- Preserving Treatment Options:
Avoiding ineffective drugs due to resistance testing safeguards a broader arsenal of therapeutic options for future use.
The Synergy of Diagnostics and Therapeutics:
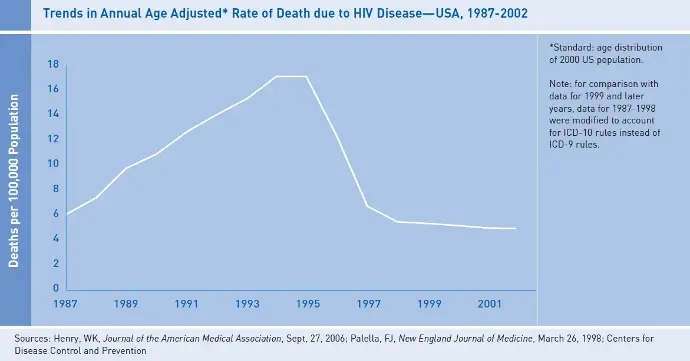
The interplay between laboratory diagnostics and antiretroviral therapy forms the bedrock of successful HIV management. Lab tests provide the crucial data for informed clinical decision-making, while ART drugs translate that information into tangible improvements in patient outcomes. This dynamic partnership has led to a significant decline in HIV-related morbidity and mortality, transforming the disease from a death sentence to a manageable chronic condition.
Conclusion:
The success story of HIV management cannot be fully told without acknowledging the often-overlooked role of laboratory diagnostics. These silent partners provide the vital information that empowers clinicians to tailor treatment strategies, ultimately leading to a longer and healthier life for individuals living with HIV. The ongoing evolution of diagnostic tools promises even greater precision in the future, further solidifying the critical role of laboratory testing in the fight against HIV.
Learn More About HIV On This Video