The increasing prevalence of antimicrobial resistance (AMR) presents a significant challenge to global public health. Traditional diagnostic methods often have limitations, leading to delays in targeted antibiotic therapy.
Limitations of Conventional Methods
Culture and susceptibility testing (CST), a common diagnostic approach, can take several days or even weeks to deliver definitive results. This delay can lead to the use of broad-spectrum antibiotics empirically, a practice that contributes to AMR development.
Rapid Diagnostics Offer Advantages
Rapid diagnostic tools (RDTs) provide a faster alternative. These technologies can identify the causative pathogen and its antibiotic resistance profile within hours, enabling swifter initiation of targeted therapy. Examples include:
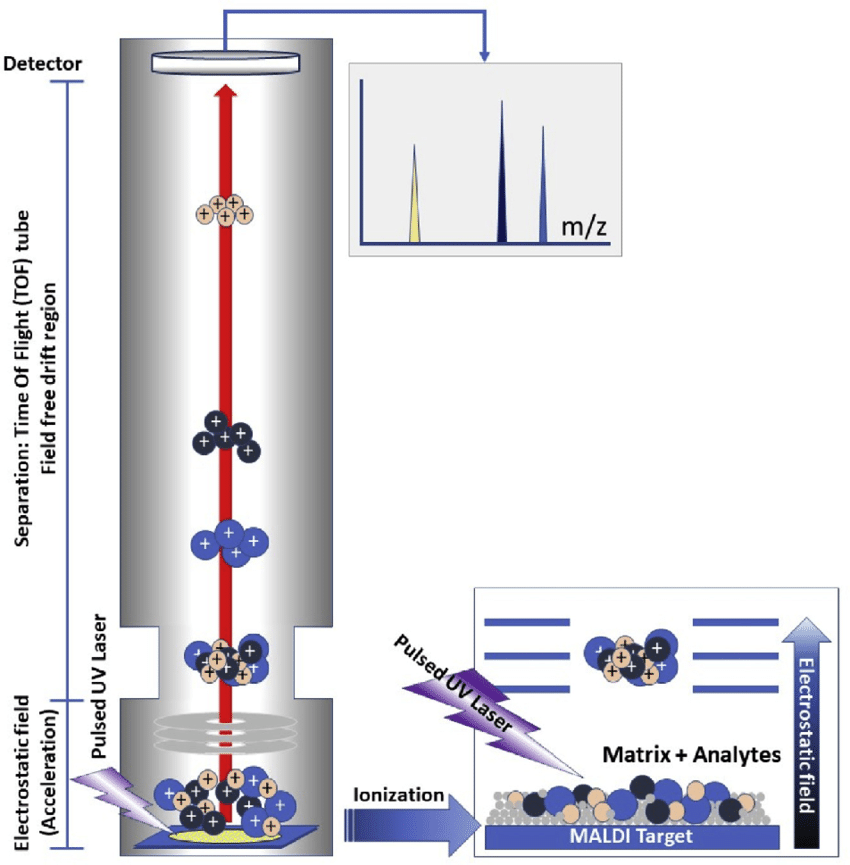
- Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS): This technique rapidly and accurately identifies bacteria based on their protein profiles.
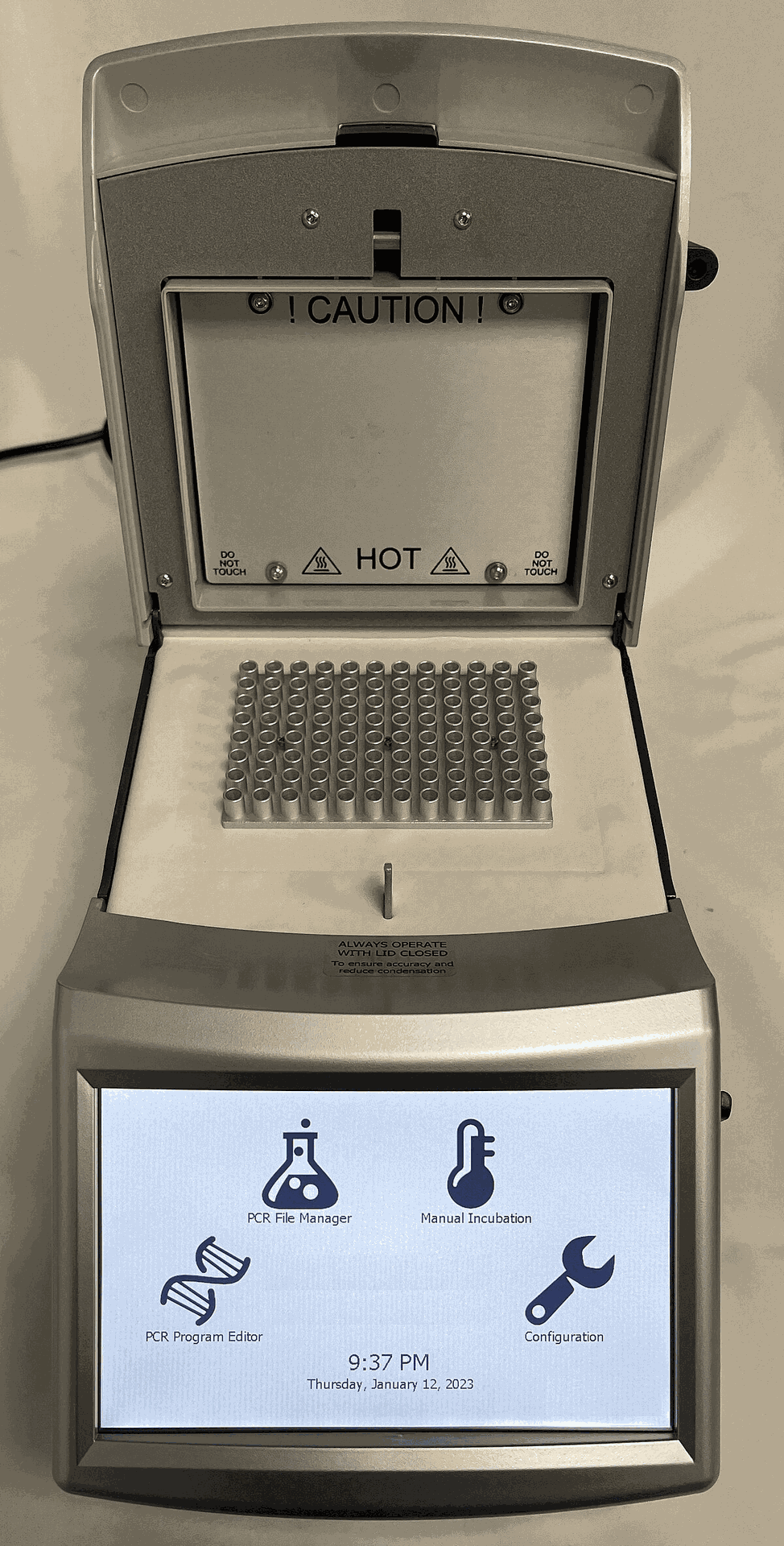
- Polymerase chain reaction (PCR)-based assays: These assays directly detect specific resistance genes in clinical samples, offering crucial information on antibiotic susceptibility.
Molecular and Point-of-Care Diagnostics
Molecular diagnostics take a deeper approach, analyzing a pathogen's genetic makeup for resistance determinants. Whole-genome sequencing (WGS) provides comprehensive insights into resistance mechanisms, informing future therapeutic strategies.
Point-of-care (POC) diagnostics are user-friendly tests designed for use outside traditional laboratory settings. These portable devices hold immense promise for resource-limited settings, enabling rapid diagnosis and treatment decisions at the point of care.
Benefits of Advanced Diagnostics
The implementation of these novel tools offers several advantages:
- Improved Patient Outcomes: Early and targeted antibiotic therapy leads to faster recovery times, fewer side effects, and improved patient outcomes.
- AMR Stewardship: Precise diagnostics promote the judicious use of antibiotics, thereby slowing the emergence of resistant strains.
- Enhanced Surveillance: Real-time data from RDTs can inform public health surveillance efforts, facilitating the tracking of emerging resistance patterns.
Challenges and Future Directions
Despite their potential, challenges remain. Standardization, cost-effectiveness, and integration into existing workflows are crucial for widespread adoption. Additionally, continuous research and development are essential to stay ahead of the evolving threat of AMR. This includes exploring novel technologies for rapid pathogen detection and targeted antimicrobial delivery.
Conclusion
Next-generation diagnostic tools offer a significant contribution to the fight against AMR. By harnessing these technologies and fostering continued innovation, we can strive towards a future where antibiotics remain effective weapons in our fight against infectious diseases.
Want to visualize how MALDI-TOF MS works? Check out this video.