Immunotherapy has revolutionized cancer treatment by leveraging the body's immune system to target and destroy cancer cells. This blog post explores the core principles of immunotherapy, outlining its various approaches and their mechanisms of action.
The Immune System: Our Defense Network
The human immune system functions as a complex network of cells, tissues, and organs that shield the body from pathogens and foreign invaders. Key components include:
- Antigen-presenting cells (APCs): These cells, like dendritic cells, capture antigens (foreign molecules) and present them to T lymphocytes, initiating an immune response.
- T lymphocytes (T cells): These are further categorized into cytotoxic T cells (CD8+ T cells) that directly eliminate target cells and helper T cells (CD4+ T cells) that coordinate the immune response.
- B lymphocytes (B cells): These cells produce antibodies, specialized proteins that bind to specific antigens, facilitating the elimination of target cells.
Immunotherapy: Reinforcing the Immune Response
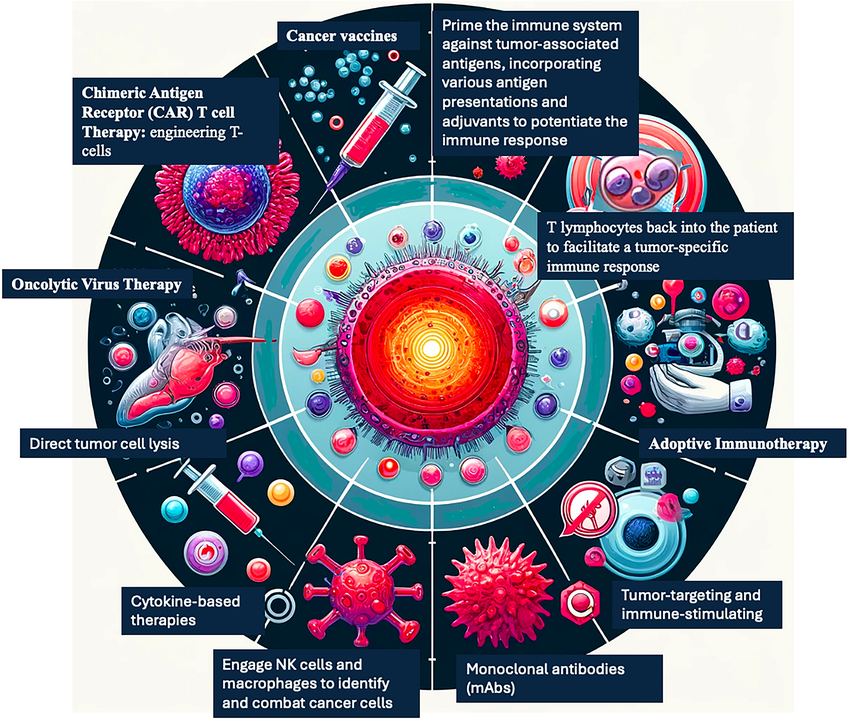
Cancer cells can evade immune detection through various mechanisms. Immunotherapy strategies aim to overcome these evasion tactics and empower the immune system to recognize and destroy cancer cells. Here are some key approaches:
- Checkpoint blockade: This strategy targets molecules (e.g., CTLA-4, PD-1) that function as immune checkpoints, naturally downregulating T cell activity to prevent autoimmune responses. Blocking these checkpoints unleashes a potent anti-tumor T cell response.
- CAR T-cell therapy: Chimeric antigen receptor (CAR) T-cell therapy involves genetically modifying a patient's T cells to express receptors that recognize specific tumor antigens. These modified T cells are then reintroduced into the patient, where they can effectively target and eradicate cancer cells.
- Cancer vaccines: These vaccines train the immune system to identify and attack cancer cells. Therapeutic cancer vaccines typically target tumor-associated antigens (TAAs) or tumor-specific antigens (TSAs) to elicit a cytotoxic T cell response.
- Cytokines: Cytokines are signaling molecules that regulate immune cell function. Immunotherapy can involve administering cytokines, such as interleukin-2 (IL-2), to stimulate the proliferation and activity of T cells and natural killer (NK) cells.
Clinical Impact and Future Directions
Immunotherapy has shown remarkable success in treating various cancers, leading to long-lasting responses and improved patient outcomes. However, challenges remain, such as optimizing treatment effectiveness for a wider range of patients and overcoming tumor heterogeneity, where tumors exhibit diverse antigen profiles. Ongoing research focuses on combination therapies with other treatment modalities, development of personalized immunotherapies, and targeting novel immune checkpoints for enhanced clinical benefit.
Reliable Reagents: Essential for Research Advancement
The field of immunotherapy is heavily reliant on cutting-edge research to develop novel therapies and improve treatment efficacy. Researchers require access to high-quality, dependable reagents for their investigations. Suppliers like Maxanim play a critical role in providing scientists with the necessary tools to unlock the full potential of immunotherapy. Maxanim offers a comprehensive portfolio of research reagents, including antibodies, cytokines, and cell culture media, ensuring researchers have the resources they need to make significant breakthroughs in this exciting area.
Conclusion
Immunotherapy represents a significant shift in cancer treatment, empowering the body's natural defense system to combat cancer. By understanding the fundamental principles and diverse approaches of immunotherapy, scientists and researchers can contribute to its continued development and application for improved patient care.
Learn More In The Following Video: